The Emma Lewis Case
The lunch rush at Harbor Diner in Atlanta was winding down on a Thursday afternoon that started like any other. Rachel Lewis wiped down tables in the back section, her worn-out sneakers squeaking against the black-and-white checkered floor. Her shift had started at six that morning, and she still had three hours to go, but seeing her daughter Emma sitting in their usual corner booth made every aching muscle worth it.
Emma, nine years old with braids tied back with pink ribbons, was doing her homework—math problems sprawled across the scratched Formica table. She’d come straight from school, her backpack still slung over her shoulder, a half-eaten grilled cheese sandwich cooling on a plate beside her textbook.
“Mama, what’s seven times eight?” Emma called out, pencil hovering over her worksheet.
“Fifty-six, baby,” Rachel answered automatically, balancing three plates on her arm as she passed. “But you need to figure out how you get there, not just the answer.”
Emma stuck her tongue out in concentration, the way she always did when thinking hard. Rachel smiled despite her exhaustion. These afternoons were their routine—had been for two years since the divorce, since James had moved out to his executive apartment downtown, since everything had changed. Emma would finish school, take the bus to the diner, do homework while Rachel finished her shift, and then they’d walk home together to their one-bedroom apartment three blocks away.
It wasn’t the life Rachel had imagined when she’d married James Lewis ten years ago, back when he was just starting his career in hospital administration, before MedCore International had promoted him to regional manager, then VP, then CEO. Back when they were a team instead of two people who’d grown into different worlds.
“Mama, I don’t feel good,” Emma said suddenly, her voice small.
Rachel turned, immediately alert to that particular tone. “What kind of not good, sweetheart?”
“My chest feels tight. Like somebody’s squeezing it.” Emma’s hand went to her sternum, her face scrunched with discomfort.
Rachel set down her tray and hurried over, pressing the back of her hand to Emma’s forehead. No fever. “Probably just ate too fast again. Take some deep breaths for me, okay?”
Emma tried, but her breathing was shallow, rapid. Her eyes were wide now, scared in a way that made Rachel’s maternal instincts scream.
“Baby, can you stand up for me?”
Emma slid out of the booth, and that’s when it happened. One moment she was standing, the next her legs buckled. She collapsed in a heap, her small body hitting the floor with a sickening thud.
“Emma!” Rachel’s scream cut through the diner’s ambient noise like a knife. Plates clattered. Customers gasped. Rachel dropped to her knees beside her daughter, whose lips were already turning a dusky blue. “Somebody call 911!”
Marcus, the cook, burst through the kitchen doors. “I’m calling now! What happened?”
“I don’t know!” Rachel’s hands shook as she turned Emma onto her side, remembering the recovery position from that CPR class she’d taken years ago. “She said her chest hurt and then she just—Emma, baby, stay with me!”
Emma’s eyes were half-open but unfocused, her breathing ragged and irregular. A thin line of drool escaped the corner of her mouth. Rachel felt for a pulse—there, but weak and fluttering like a trapped bird.
The ambulance took eleven minutes to arrive—Rachel counted every second. But she couldn’t wait. By the seventh minute, she’d already scooped Emma into her arms and was running.
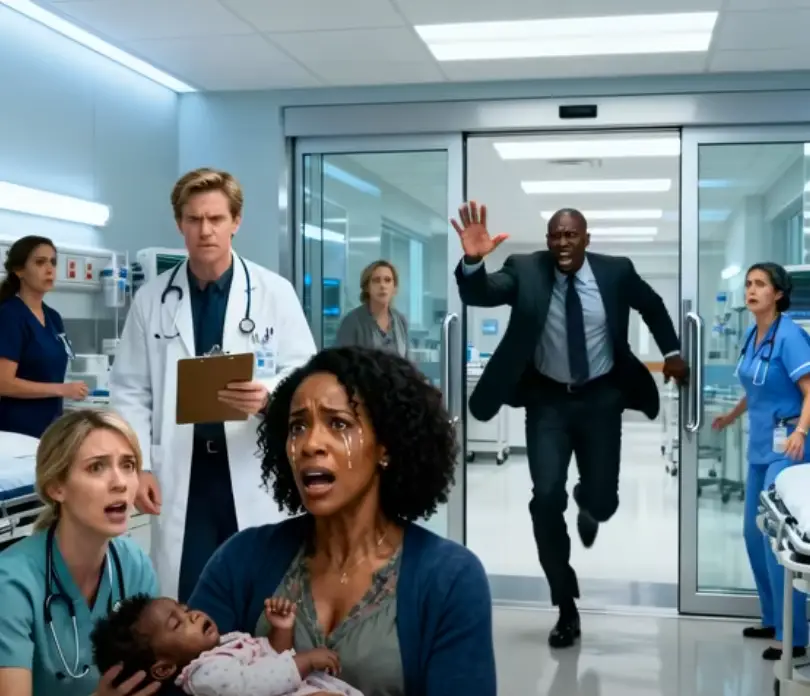
St. Matthew’s Hospital was only four blocks away. Rachel had passed it a thousand times on her way to work, never imagining she’d burst through those automatic doors with her dying child in her arms, her server’s apron still tied around her waist, her voice raw from screaming.
“Please! My daughter—she’s not breathing right! She collapsed!”
The emergency department was moderately busy for a Thursday afternoon. Two elderly patients sat in wheelchairs near the triage desk. A man with a bandaged hand filled out paperwork. A child’s cartoon played on a mounted television in the corner.
Behind the front desk, Dr. Henry Wallace looked up from his computer screen with the expression of a man deeply annoyed by the interruption. He was in his late forties, with silver hair carefully combed back and reading glasses perched on his nose. His white coat was crisp, spotless, the epitome of professional authority.
His eyes flicked over Rachel—taking in her stained apron, her faded jeans, her dark skin glistening with sweat and tears. Something shifted in his expression, something Rachel couldn’t quite name but felt in her bones.
“Do you have insurance?” he asked, his voice flat and bureaucratic.
Rachel froze. The question hung in the air like poison gas. “What?”
“Insurance, ma’am. Your insurance card. Or another valid payment method.”
“She’s nine years old!” Rachel’s voice cracked with desperation. “Please, she’s dying! Look at her!”
Emma’s chest rose and fell in shallow, irregular gasps. Her skin had taken on a grayish tone, her lips darkening from blue to purple.
Dr. Wallace glanced at Emma with what could only be described as clinical detachment. “I understand you’re upset, but we have protocols. We need to complete registration before we can begin treatment. There are rules for a reason.”
The triage nurse, Megan Ruiz, a woman in her early thirties with kind eyes and auburn hair pulled back in a practical ponytail, looked up from her station with unconcealed horror.
“Dr. Wallace, this is clearly an emergency situation. The child is cyanotic! We need to—”
“Nurse Ruiz,” Wallace interrupted, his voice sharp, “protocol dictates that we complete registration before admitting patients to treatment areas. I don’t make exceptions, regardless of the circumstances. We’ve had too many billing issues this quarter.”
“Billing issues?” Rachel’s voice rose to a shriek. “My daughter is DYING!”
Emma’s small body began to convulse in Rachel’s arms. Her tiny hands twitched, fingers curling and uncurling. Her eyes rolled back, showing only whites. Foam appeared at the corner of her mouth.
“Put her down,” Nurse Megan said urgently, rushing around the desk. “Put her on the floor, ma’am. Now!”
Rachel lowered Emma onto the cold linoleum, her hands shaking so badly she could barely control her movements. Tears streamed down her face, dropping onto her daughter’s still form.
“Please,” Rachel begged, looking up at Dr. Wallace. “Please, I’m begging you. I’ll pay whatever you want. I’ll sign anything. Just help her!”
Wallace’s jaw tightened. He looked at Rachel, then at Emma, then at the computer screen where the registration form sat incomplete. “Get her insurance information first,” he told the receptionist, a nervous young woman named Bethany who looked like she wanted to disappear into the floor. “Then we’ll see what we can do.”
“See what we can do?” Nurse Megan’s voice was incredulous. “Dr. Wallace, if we wait another minute, this child could have permanent brain damage or die. We need to intubate now!”
“You will wait for proper authorization,” Wallace snapped, his voice cold as ice. “If you touch that patient without completing registration, you’re violating hospital policy. Do you want to lose your license over this?”
The seconds ticked by like hours. Emma’s convulsions were getting worse. Her back arched off the floor. Foam and saliva bubbled from her mouth.
Nurse Megan looked at Wallace, then at Emma, then back at Wallace. Something hardened in her expression—a decision being made in real-time. She tore off her gloves with sharp, decisive movements.
“I don’t care about hospital policy,” she said quietly. “I care about saving lives.”
She dropped to her knees beside Emma and began chest compressions, her hands positioned precisely over the child’s sternum. “One, two, three, four,” she counted under her breath, pressing rhythmically. “Hang in there, sweetheart. Stay with me.”
“STOP THIS MADNESS!” Wallace roared, storming toward her, his face flushed red with rage. “Nurse Ruiz, I am ordering you to stop immediately! You are in violation of—”
The automatic entrance doors burst open with such force they slammed against the wall.
A tall man in a dark gray suit strode in, his expensive leather shoes clicking sharply against the floor. His tie was loosened, his jaw set, his eyes wild with panic. His voice boomed through the emergency department like thunder:
“WHERE IS MY DAUGHTER?”
The security guard stepped back instinctively. Staff members froze mid-motion. Patients in the waiting room stared. Everyone who worked at St. Matthew’s Hospital recognized that voice, that face, that commanding presence.
James Lewis. CEO of MedCore International, the massive healthcare corporation that owned St. Matthew’s Hospital along with forty-three other medical facilities across the Southeast.
His eyes swept the room and landed on the scene unfolding on the floor—a nurse performing chest compressions on a small Black girl while a woman in a server’s apron sobbed beside them. For a split second, his executive mask remained in place. Then recognition hit him like a physical blow.
“Emma?” His voice broke on his daughter’s name. “EMMA!”
He crossed the distance in three long strides, dropping to his knees beside Rachel. “What happened? Why isn’t she—” His eyes went to the crash cart sitting unused ten feet away, to the oxygen equipment hanging on the wall, to Dr. Wallace standing frozen by the nurses’ station.
“They wouldn’t help her,” Rachel sobbed, grabbing James’s arm. “They asked for money first—insurance cards and payment—while she was dying, James! They just stood there!”
James’s face went through a series of transformations—shock, disbelief, and finally, a cold fury that made the air in the room feel twenty degrees colder.
He stood up slowly, his six-foot-three frame seeming to tower over everyone present. When he spoke, his voice was dangerously calm, the kind of quiet that precedes a hurricane.
“I want to know,” he said, enunciating each word with crystal clarity, “why my daughter has been lying on this floor, not breathing properly, while your staff argues about paperwork.”
Dr. Wallace’s face had gone from red to white in the span of seconds. “Mr. Lewis, I—I didn’t realize—”
“You didn’t realize she was my daughter,” James said, his voice dropping even lower. “Let me be very clear about what you’re saying. You didn’t help a nine-year-old child who was clearly in medical distress because you didn’t recognize her as someone important. Is that correct?”
“No, sir, that’s not—I was following protocol—”
“Protocol.” James turned to look at Emma, who was now surrounded by a full emergency team that had materialized the moment his identity became clear. An oxygen mask covered her small face. IV lines were being inserted. The crash cart had been wheeled over. “Tell me, Dr. Wallace, what protocol allows you to watch a child turn blue and do nothing?”
Wallace opened his mouth, closed it, opened it again. No words came out.
“Get him out of my sight,” James said quietly to the hospital security. “And someone find the director. Now.”
The next three hours were a blur of controlled chaos. Emma was rushed to the intensive care unit. A full code team worked on her—intubation, medications, continuous monitoring. James and Rachel sat together in the ICU waiting room, not quite touching but united in their terror.
“She said her chest hurt,” Rachel whispered, staring at her hands. “I thought it was nothing. Just indigestion from eating too fast.”
“This isn’t your fault,” James said firmly.
“I was working, James. Our daughter collapsed while I was working because I can’t afford childcare and—”
“Stop.” He took her hand, something they hadn’t done in over a year. “None of that matters right now. What matters is that she gets better.”
Dr. Sarah Chen, the head of pediatric intensive care, emerged from the ICU at 6:47 PM. Her expression was carefully neutral, the mask of a doctor who’d delivered both good news and devastating news too many times to count.
“She’s stable,” Dr. Chen said, and both parents released breaths they didn’t know they’d been holding. “We’ve diagnosed a severe allergic reaction—anaphylaxis—likely triggered by something she ate. The delay in treatment caused significant distress to her system, but we believe we caught it in time. However, she’ll need to remain in intensive care for at least forty-eight hours for monitoring.”
“Can we see her?” Rachel asked, her voice hoarse.
“Of course. But I need to prepare you—she’s on a ventilator. She looks fragile. It’s frightening, but it’s helping her breathe while her body recovers.”
Emma looked impossibly small in the hospital bed, surrounded by machines that beeped and hummed. Tubes ran from her arms. A ventilator whooshed rhythmically, breathing for her. Rachel broke down completely, her sobs echoing off the sterile walls.
James stood rigid, his hands clenched into fists. “Who else knows about what happened downstairs?”
“Sir, I think right now—”
“Who else knows?” James’s voice was steel.
Dr. Chen hesitated. “The entire emergency department staff. Security. And I believe one of the patients in the waiting room was filming on their phone.”
The video hit Twitter at 11:43 PM that night.
The person who’d filmed it—a college student named Marcus Tanner who’d been waiting to be treated for a sprained ankle—had initially thought nothing of it. Just another unfortunate incident at an overcrowded emergency room. But when he got home and actually watched the footage, when he saw the timestamp showing how long that little girl had lain on the floor, when he heard the doctor explicitly refuse treatment until payment was confirmed, something in him snapped.
He posted it with a simple caption: “Doctor refuses to treat Black child until insurance is confirmed. This happened TODAY at St. Matthew’s Hospital in Atlanta. Her father had to arrive and identify himself as the CEO of the hospital’s parent company before they would help her. She almost DIED. This is America’s healthcare system.”
By 2 AM, the video had 50,000 views.
By 6 AM, 500,000.
By noon the next day, it had been viewed over five million times.
The footage was devastating in its clarity. The audio captured everything—Rachel’s desperate pleas, Wallace’s cold refusals, Megan’s defiant choice to help anyway, and finally, James’s explosive arrival and the sudden mobilization of the entire emergency team.
“Justice for Emma” began trending on Twitter.
“Dr. Wallace” trended on Twitter.
“St. Matthew’s Hospital” trended on Twitter.
The hospital’s phone lines were overwhelmed. Protesters gathered outside by 8 AM—first a dozen, then fifty, then hundreds. They held signs reading “Patients, Not Profits” and “Black Lives Matter in Healthcare Too” and “Emma Lewis Deserves Justice.”
News vans from every major network parked outside the hospital. Reporters ambushed staff members leaving their shifts. Dr. Wallace’s photo circulated everywhere—his professional headshot from the hospital website, his LinkedIn profile, pictures from a medical conference he’d attended three months earlier.
And then the other stories started coming out.
A Twitter thread from a former patient: “Dr. Wallace treated me at St. Matthew’s last year. He literally asked if I could afford an X-ray before he’d even examine my broken arm. I’m a Black woman. I filed a complaint. Nothing happened.”
A Facebook post: “My mother went to that ER two years ago with chest pain. Wallace made her wait in the lobby for THREE HOURS while he treated white patients who came in after her. She ended up having a heart attack in the waiting room.”
A Reddit thread: “I’m a medical student who did a rotation at St. Matthew’s. Wallace was openly racist. He would make comments about ‘those people’ not having insurance and ‘being a drain on the system.’ Multiple students reported him. Nothing ever happened.”
The floodgates had opened.
By day three, the Georgia State Medical Board announced a formal investigation. The hospital board convened an emergency meeting. Civil rights organizations called for Wallace’s immediate termination. MedCore International’s stock price began to drop.
James refused to comment publicly. “This isn’t about me,” he told reporters who ambushed him outside the hospital. “This is about a system that allowed my daughter’s life to depend on someone’s snap judgment about her worth based on her mother’s appearance. This is about a system where the color of our skin determined whether she lived or died.”
Emma woke up on the fourth day. The ventilator had been removed twelve hours earlier, and she’d been breathing on her own since. Rachel was asleep in the chair beside her bed when Emma’s small voice croaked out a single word:
“Mama?”
Rachel’s eyes flew open. “Baby! Oh, thank God. Baby, I’m right here.”
“What happened? Where am I?”
“You’re in the hospital, sweetheart. You had an allergic reaction. But you’re going to be okay. You’re going to be just fine.”
Emma’s eyes filled with tears. “The man wouldn’t help me. I remember him saying no.”
Rachel’s jaw clenched. “I know, baby. I know.”
Dr. Henry Wallace was officially terminated on day seven. The hospital board had met in emergency session for six hours. The evidence was overwhelming—not just the video, but testimony from other staff members, documentation of previous complaints that had been ignored, and the undeniable fact that his actions had nearly killed a child.
His termination letter was terse: “Dr. Henry Wallace is no longer employed by St. Matthew’s Hospital or any facility within the MedCore International healthcare system. His actions violated both hospital policy and fundamental medical ethics.”
Wallace appeared on a local news station two days later, his first and only public statement. He sat in his home office, surrounded by his medical degrees and certifications, his face haggard and defiant.
“This has been blown completely out of proportion,” he said. “I followed standard hospital protocol regarding patient registration. The fact that the girl’s father happens to be a powerful executive doesn’t change that. I was following the rules.”
The interviewer, a sharp-eyed journalist named Patricia Moore, leaned forward. “Dr. Wallace, the child was turning blue. She was convulsing. Multiple witnesses say you explicitly refused to allow treatment until insurance was confirmed. How is that following protocol?”
“Emergency departments across this country deal with patients who can’t or won’t pay every single day. If we treated everyone without confirming ability to pay, hospitals would go bankrupt. There has to be a process.”
“Even when a child is dying?”
Wallace’s jaw tightened. “The system isn’t perfect, but I was operating within established guidelines.”
“Let me ask you directly: Do you believe race played any role in your decision?”
“Absolutely not. I treat all patients the same.”
“Then why did multiple staff members and witnesses report that you specifically commented on the mother’s appearance—her clothing, her job as a server—before refusing treatment?”
“That’s hearsay. I don’t recall making any such comments.”
The interview went viral for all the wrong reasons. Wallace’s defensive posture, his refusal to apologize, his insistence that he’d done nothing wrong—it all reinforced the public’s fury. His medical license was suspended pending investigation. His home address was doxxed online. He received death threats. He had to hire private security.
Meanwhile, Nurse Megan Ruiz became a folk hero. Interview requests flooded in. A GoFundMe to support her raised over $200,000 in donations. James personally called her to express his gratitude.
“You saved my daughter’s life,” he said, his voice thick with emotion. “You risked your career to do what was right.”
“I didn’t think about it like that,” Megan said quietly. “I just… I couldn’t stand there and watch a child die because of paperwork. I couldn’t do it.”
“You’re a hero.”
“I’m just a nurse who remembered why I went into medicine.”
Three months later, the “Emma Lewis Initiative” was officially launched at a press conference held on the grounds of St. Matthew’s Hospital. The crowd was massive—reporters, hospital staff, community members, civil rights leaders, and politicians.
The initiative was comprehensive:
- Immediate treatment protocols: No patient in a clear medical emergency could be denied initial stabilizing treatment, regardless of insurance status or ability to pay.
- Bias training: Mandatory anti-racism and implicit bias training for all healthcare workers, with regular refresher courses.
- Anonymous reporting: A hotline for staff to report discriminatory practices without fear of retaliation.
- Financial support: A $50 million fund to cover emergency care for uninsured patients.
- Community oversight: A board composed of community members who would review emergency department practices quarterly.
Emma stood between her parents at the ceremony, wearing a yellow dress and holding a teddy bear nearly as big as she was. She’d regained her strength and her spark. The media loved her—this brave little girl who’d become the face of healthcare reform.
James addressed the crowd first, his voice strong but emotional. “I’m not here as a CEO today. I’m here as a father who watched his daughter almost die because someone looked at her and made assumptions based on the color of her skin and her mother’s appearance. I’m here as someone who had the resources and the power to demand justice—and that shouldn’t be what it takes. Every child deserves the same immediate care that Emma received once I walked through those doors. Every parent deserves to have their child’s life valued.”
Rachel spoke next, her voice quieter but no less powerful. “Change doesn’t start in the law books or the boardrooms. It starts when one person decides to care enough to act—like Nurse Megan did that day. It starts when we look at each other and see human beings instead of statistics or dollar signs. It starts when we remember that behind every patient is a family, a story, a life that matters.”
Megan stood nearby, tears streaming down her face as the crowd erupted in applause.
The initiative didn’t just change St. Matthew’s Hospital. Within a year, over 200 hospitals across twelve states had adopted similar protocols. Medical schools added new courses on healthcare equity and implicit bias. The phrase “The Emma Lewis Case” became a staple in medical ethics classes across the country—not just as a cautionary tale, but as a catalyst for change.
The Georgia State Medical Board revoked Dr. Wallace’s license after a six-month investigation. The final report was damning: “Dr. Henry Wallace demonstrated a pattern of discriminatory behavior that violated both the ethical standards of medical practice and the fundamental principle that all patients deserve equal care. His actions on the day in question were not an isolated incident but part of a broader pattern of bias that had no place in medicine.”
At his final disciplinary hearing, Wallace remained defiant. “I was following protocol,” he insisted. “The system failed, not me.”
But the board’s chairperson, Dr. Amelia Foster, an elderly Black woman who’d practiced medicine for forty years, wasn’t having it.
“Dr. Wallace, you had a choice. When you saw that child, you could have chosen to see a human being in distress. Instead, you chose to see a problem, a potential liability, a billing issue. You looked at her mother and made assumptions about her ability to pay based on her appearance and her race. Don’t insult this board’s intelligence by pretending otherwise.”
“With all due respect—”
“No,” Dr. Foster interrupted. “You don’t get to invoke respect. Respect is earned through actions, and your actions demonstrated a fundamental lack of respect for human life. The medical profession is built on a simple promise: to do no harm. You broke that promise in the most egregious way possible. Medicine is not a privilege for the wealthy or the well-connected. It is a duty to all humanity. You forgot that duty, and now you’ll face the consequences.”
The final statement from the board read: “Dr. Henry Wallace’s medical license is permanently revoked. He is prohibited from practicing medicine in any capacity within the state of Georgia. This decision is final and not subject to appeal.”
Two years after the incident, the Lewis family gathered for Emma’s eleventh birthday party at their home. The divorce had been finalized, but James and Rachel had found a new kind of partnership—not as spouses, but as co-parents united in protecting their daughter and working to ensure what happened to her never happened to anyone else.
Emma blew out her candles, surrounded by friends and family. She was thriving—healthy, happy, advocating for healthcare reform alongside her parents. She’d spoken at conferences, met with legislators, and become a powerful voice for change.
That night, after the guests had left and the cake was put away, Rachel tucked Emma into bed. The little girl looked up with the same curious eyes that saw too much and understood too well.
“Mama,” she whispered, “why do you think the doctor didn’t want to help me?”
Rachel had known this question would come eventually. She’d prepared for it, rehearsed answers in her mind. But now, facing her daughter’s innocent gaze, all the prepared speeches fell away.
“Because some people,” she said gently, brushing Emma’s braids back from her forehead, “forget to see the person in front of them. They see skin color, or clothes, or things that don’t matter. They forget that every person deserves kindness and care.”
“But he was a doctor. Isn’t he supposed to help people?”
“He was supposed to, yes. And most doctors do. Most people in the world are good, baby. But sometimes, people let their fears or their prejudices make them do bad things.”
Emma was quiet for a moment, processing. “Do you think he’s sorry?”
Rachel thought about Wallace’s defiant interviews, his refusal to apologize, his insistence that he’d done nothing wrong. “I don’t know, sweetheart. I hope one day he will be.”
“I’m not sorry it happened,” Emma said suddenly.
Rachel pulled back, surprised. “What do you mean?”
“I mean, it was scary and it hurt. But now other kids won’t have to go through what I did. Right? That’s what the Initiative does. It helps people.”
Rachel’s eyes filled with tears. “Yes, baby. That’s exactly what it does.”
“Then maybe,” Emma said, her voice growing sleepy, “maybe it happened for a reason. So other kids don’t get hurt. So things can change.”
Rachel sat there long after Emma fell asleep, watching her daughter’s chest rise and fall with the steady rhythm of healthy breathing. She thought about that day in the hospital, about Nurse Megan’s courage, about James’s fury, about the video that had sparked a movement.
Outside their window, Atlanta glowed softly in the summer night—a city changed forever by a little girl who almost didn’t make it, and the people who refused to let her story be forgotten.
The Emma Lewis Initiative continued to grow. It expanded to all fifty states within five years. Emma herself eventually went to medical school, determined to be the kind of doctor who saw people first and everything else second. Nurse Megan Ruiz was promoted to Director of Emergency Services at St. Matthew’s, where she trained a new generation of healthcare workers in compassionate, equitable care.
As for Dr. Henry Wallace, he disappeared from public life. Some said he left Georgia, moved to a small town where nobody knew his name or his history. Others said he spent his days bitter and resentful, convinced he’d been unfairly targeted. The truth was, nobody really cared what happened to him anymore.
The world had moved on.
It had changed.
And it had changed because one nurse chose courage over compliance, one father used his privilege to demand justice, one mother refused to be silent, and one little girl’s near-death became a catalyst for transformation.
That’s the story of Emma Lewis—not just of what was done to her, but of what she inspired, of how a moment of crisis became a movement, of how one child’s suffering led to healing for thousands.
Her legacy wasn’t written in the emergency room that day.
It was written in every emergency room that followed, in every child treated immediately and without question, in every healthcare worker who remembered to see the human before the paperwork.
That’s the real story.
And it’s still being written today.

Lila Hart is a dedicated Digital Archivist and Research Specialist with a keen eye for preserving and curating meaningful content. At TheArchivists, she specializes in organizing and managing digital archives, ensuring that valuable stories and historical moments are accessible for generations to come.
Lila earned her degree in History and Archival Studies from the University of Edinburgh, where she cultivated her passion for documenting the past and preserving cultural heritage. Her expertise lies in combining traditional archival techniques with modern digital tools, allowing her to create comprehensive and engaging collections that resonate with audiences worldwide.
At TheArchivists, Lila is known for her meticulous attention to detail and her ability to uncover hidden gems within extensive archives. Her work is praised for its depth, authenticity, and contribution to the preservation of knowledge in the digital age.
Driven by a commitment to preserving stories that matter, Lila is passionate about exploring the intersection of history and technology. Her goal is to ensure that every piece of content she handles reflects the richness of human experiences and remains a source of inspiration for years to come.